Table of Contents:
- The Problem: Why Whitening Promises Fail
- What to Consider: Understanding Tooth Color and Whitening Chemistry
- How to Choose: Selecting Appropriate Treatment and Concentration
- MD Spa’s Professional Whitening Excellence
- Frequently Asked Questions
The Problem: Why Whitening Promises Fail
The Shade Guide Deception Crisis
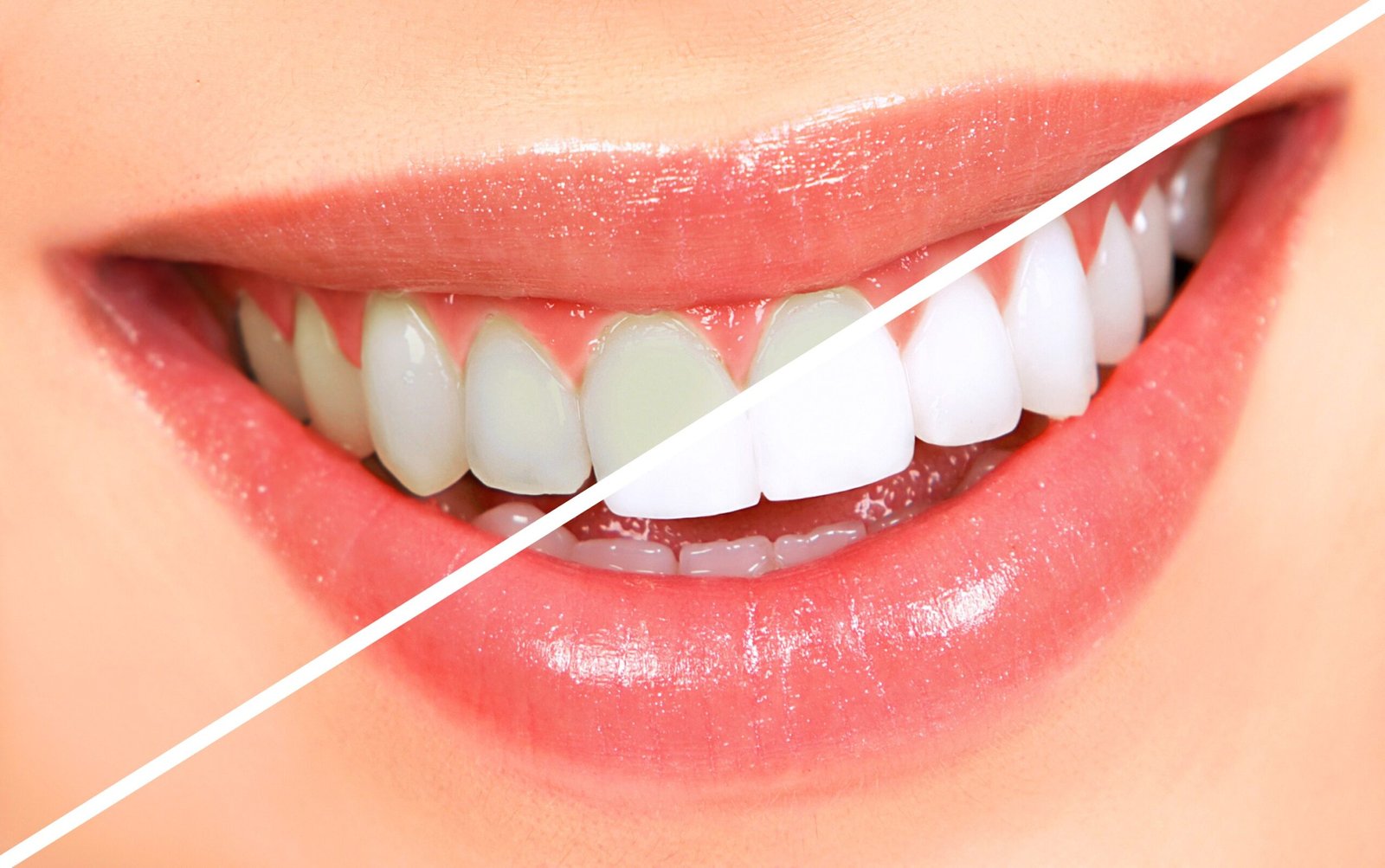
The dental shade guide system gets weaponized for marketing purposes, with 74% of whitening advertisements promising unrealistic shade improvements that natural teeth cannot achieve without causing permanent damage. Providers show B1 or “Hollywood white” as standard results when most teeth start at A3-A4 and can only safely lighten 2-5 shades. Shade guides designed for matching dental restorations get misused for whitening assessment. Before-after photos use different lighting, angles, and color correction. This systematic deception creates impossible expectations, guaranteeing patient disappointment when biological limits prevent achieving marketed results. The VITA shade guide wasn’t designed for whitening assessment, yet gets universally misapplied creating confusion about realistic outcomes. The guide arranges shades by hue (color family) not brightness, making linear improvement tracking impossible. A3 to B2 might represent lightening despite different letter designation. Natural teeth rarely match any single shade tab perfectly. Multiple guides exist with inconsistent numbering. According to dermatology research, proper whitening assessment requires spectrophotometer measurement, not subjective shade matching, yet most providers rely on inaccurate visual comparison.Shade guide manipulation tactics:
- Comparing dehydrated teeth (appear whiter temporarily)
- Using bleached shade guides beyond natural range
- Digital whitening in before-after photos
- Different lighting making teeth appear lighter
- Showing denture white as achievable goal
- Ignoring individual variation in whitening potential
The Peroxide Percentage Arms Race
Whitening products engage in concentration escalation with 35%, 44%, even 60% hydrogen peroxide marketed as providing superior results, when research shows concentrations above 10% hydrogen peroxide provide no additional whitening while exponentially increasing sensitivity and enamel damage. Higher concentrations work faster, not better, reaching the same endpoint with more pain. Carbamide peroxide percentages confuse consumers since 35% carbamide equals only 12% hydrogen peroxide. This percentage manipulation tricks patients into damaging treatments that could achieve identical results gently. The chemistry of tooth whitening involves peroxide breaking down into free radicals that penetrate enamel and oxidize chromophore molecules. This process reaches saturation point where additional peroxide provides no benefit. Studies demonstrate 10% hydrogen peroxide achieves maximum whitening—higher concentrations only increase side effects. Yet providers push extreme concentrations claiming superior results, when they’re simply causing unnecessary trauma for identical outcomes. The treatment safety protocols confirm optimal whitening occurs at moderate concentrations with extended contact time, not aggressive quick treatments.Peroxide concentration reality:
- 3-6% hydrogen peroxide: Effective for gradual whitening
- 10% hydrogen peroxide: Maximum effective concentration
- 15-20%: Faster but not whiter, more sensitivity
- 25-35%: Significant enamel damage risk
- Above 35%: Dangerous with no additional benefit
- Carbamide peroxide: Divide by 3 for hydrogen equivalent
The LED Light and Accelerator Scam
LED lights, UV lamps, and “accelerator” treatments add $100-$300 to whitening costs while providing zero additional whitening according to multiple clinical studies, representing pure profit margin through technological theater. Blue LED lights cannot generate heat necessary for peroxide acceleration. UV light poses cancer risks without whitening benefits. “Laser” whitening uses conventional bleaching with expensive equipment for show. These devices create perception of advanced treatment while the peroxide does all actual work, deceiving patients into paying premium for placebo technology. The original light-activated whitening used specific wavelengths with photosensitizers requiring precise chemistry. Modern “light-accelerated” systems use standard peroxide with decorative lights providing no chemical activation. Studies comparing peroxide alone versus peroxide with LED show identical results. Temperature measurements confirm LED devices don’t generate sufficient heat for acceleration. Yet providers charge hundreds extra for theatrical light shows contributing nothing to outcomes. According to aesthetic medicine guidelines, light activation represents outdated technology replaced by optimized peroxide formulations.Light/accelerator deception methods:
- Blue LED lights (no chemical effect)
- UV lamps (dangerous, ineffective)
- “Laser” whitening (misleading terminology)
- Heat lamps (damage risk, minimal benefit)
- “Plasma arc” devices (marketing nonsense)
- “Zoom” lights (standard peroxide doing work)
The Sensitivity Cover-Up Pattern
Tooth sensitivity affects 67% of whitening patients with 23% experiencing severe pain requiring treatment discontinuation, yet providers dismiss this as minor temporary discomfort while failing to explain mechanisms or provide adequate management. Sensitivity results from peroxide penetrating through enamel to dentin, causing fluid movement in dentinal tubules that triggers nerve responses. Higher concentrations cause more severe sensitivity lasting weeks to months. Some patients develop irreversible pulpal damage. This predictable consequence gets minimized to avoid deterring treatment sales. The mechanism of whitening-induced sensitivity involves multiple pathways providers never explain. Peroxide causes enamel demineralization increasing porosity. Dentinal tubules become exposed and widened. Pulpal inflammation develops from chemical irritation. Nerve sensitization lowers pain thresholds. Reversible pulpitis may progress to irreversible damage. These serious biological responses get dismissed as “normal” when representing concerning tissue trauma that proper protocols could minimize.Sensitivity mechanisms and timeline:
- During treatment: Direct chemical irritation
- 0-24 hours: Peak nerve stimulation
- Days 1-3: Continued inflammation
- Days 4-7: Gradual reduction
- Weeks 2-4: Resolution in most
- Permanent: 5-10% of aggressive cases
What to Consider: Understanding Tooth Color and Whitening Chemistry
Natural Tooth Color Determinants
Tooth color results from complex interaction of enamel thickness, dentin shade, and light properties that create individual variation in whitening potential regardless of treatment aggressiveness. Enamel acts as translucent layer over yellow dentin—thicker enamel appears whiter by masking dentin. Dentin color ranges from yellow to gray based on genetics. Light scattering through enamel crystals affects perceived brightness. These structural factors determine both starting shade and maximum achievable whitening that no amount of peroxide can exceed. Enamel thickness varies by tooth position, age, and genetics creating different whitening responses across the smile. Central incisors have thickest enamel appearing whitest. Canines show more dentin appearing yellower. Lateral incisors fall between. Age-related enamel thinning reveals more dentin. Genetic variation creates 2-fold thickness differences. This anatomical reality means uniform ultra-white results remain impossible—teeth whiten relative to their structure, not to absolute standard.Tooth color factors:
- Enamel thickness (0.5-2.5mm variation)
- Dentin color (genetic determination)
- Pulp size (affects color transmission)
- Mineralization degree (affects translucency)
- Internal structure (affects light properties)
- Age-related changes (cumulative effects)
Peroxide Chemistry and Mechanisms
Hydrogen peroxide whitening works through oxidation-reduction reactions breaking down chromophore molecules that create tooth discoloration, with effectiveness depending on concentration, pH, contact time, and temperature rather than lights or accelerators. H₂O₂ dissociates into hydroxyl radicals (HO•) and perhydroxyl ions (HOO⁻). These reactive species penetrate enamel reaching chromophores. Carbon double bonds in stain molecules break forming smaller, colorless fragments. The process continues until chromophores fragment below visible spectrum or peroxide depletes. Carbamide peroxide (CH₆N₂O₃) provides sustained release of hydrogen peroxide, breaking down into urea and hydrogen peroxide at roughly 3:1 ratio. A 30% carbamide peroxide yields 10% hydrogen peroxide over time. Slower release means longer contact time required but less sensitivity. Urea elevates pH improving stability and penetration. This controlled release makes carbamide peroxide ideal for overnight trays despite lower instantaneous concentration. According to treatment safety protocols, carbamide peroxide achieves equivalent whitening with better tolerance than hydrogen peroxide.Peroxide chemistry facts:
- Hydrogen peroxide: Direct, rapid action
- Carbamide peroxide: Slow release, gentler
- Optimal pH: 8.5-10.5 for stability
- Temperature effect: 10°C rise doubles rate
- Contact time: More important than concentration
- Saturation point: Beyond which no benefit
Enamel and Dentin Effects
Whitening affects tooth structure beyond color change, causing measurable alterations in enamel morphology, composition, and properties that providers rarely discuss. Peroxide causes enamel demineralization reducing microhardness 20-50% immediately post-treatment. Surface roughness increases facilitating restaining. Protein matrix degrades affecting structural integrity. While remineralization occurs over weeks, repeated aggressive whitening causes cumulative damage. These structural changes represent necessary evil for whitening, not benign cosmetic treatment. Scanning electron microscopy reveals enamel surface changes invisible to naked eye but significant for tooth health. Normal enamel shows smooth crystalline surface. Post-whitening shows erosion patterns, increased porosity, and crystal dissolution. Higher concentrations cause deeper alterations. Multiple treatments create cumulative effects. Remineralization partially reverses changes but never completely restores original structure. The skin aging science documents permanent enamel alterations from aggressive whitening explaining increased cavity susceptibility in frequent whiteners.Enamel effects from whitening:
- Decreased microhardness (temporary)
- Increased surface roughness
- Improve porosity
- Protein matrix degradation
- Crystal dissolution patterns
- Reduced fracture resistance
Individual Variation Factors
Whitening response varies dramatically between individuals based on genetics, age, diet, habits, and tooth structure that standardized protocols ignore. Genetic factors determine enamel thickness, dentin color, and chromophore types affecting both starting point and endpoint. Young patients with thick enamel achieve better results. Dietary chromogens from coffee, wine, curry create different stain types. Smoking stains respond differently than food stains. These variations mean identical treatment produces 5-fold differences in shade improvement. Genetic polymorphisms affect whitening through multiple pathways rarely considered. Enamel formation genes determine thickness and quality. Dentin genes control underlying color. Saliva composition affects remineralization. Drug metabolism impacts fluoride or tetracycline incorporation. Pain perception varies 10-fold between individuals. According to clinical skincare research, genetic testing could predict whitening response and sensitivity risk, though remains impractical clinically.Individual variation factors:
- Genetic enamel/dentin traits
- Age (younger better response)
- Diet (chromogen exposure)
- Habits (smoking, coffee)
- Medications (tetracycline, fluoride)
- Saliva (buffering, remineralization)
How to Choose: Selecting Appropriate Treatment and Concentration
Professional vs At-Home Decision Framework
Choosing between professional and at-home whitening depends on starting shade, sensitivity history, timeline, and budget, with professional treatment offering faster results at higher cost while at-home provides gradual whitening with better sensitivity control. Professional treatments use 15-35% hydrogen peroxide achieving noticeable results in single visit. At-home systems use 3-10% hydrogen peroxide or 10-22% carbamide peroxide over weeks. Both reach similar endpoints—professional gets there faster with more discomfort. Neither surpasses biological whitening limits regardless of marketing claims. In-office whitening suits patients wanting immediate results for events, requiring 60-90 minute appointments with noticeable improvement. Higher concentrations penetrate quickly oxidizing chromophores. Isolation prevents gum irritation. Monitoring ensures safety. Results visible immediately though partially from dehydration. True results appear after rehydration in 24-48 hours. Cost ranges $400-$800 per session with most needing 1-3 sessions. According to dermatology research, in-office achieves 2-5 shade improvement average, not 8-10 shades advertised.Professional vs at-home comparison:
- Speed: Professional 1-3 sessions, home 2-6 weeks
- Comfort: Home better, professional more sensitivity
- Cost: Professional $400-$800, home $100-$400
- Convenience: Home flexible, professional scheduled
- Results: Similar endpoints, different timeline
- Maintenance: Both require touch-ups
Concentration Selection Guidelines
Optimal peroxide concentration balances efficacy with sensitivity, as higher concentrations don’t whiten better—just faster with more pain—making moderate concentrations with extended contact superior approach. Research consistently shows 10% hydrogen peroxide or 15-20% carbamide peroxide achieves maximum whitening. Higher concentrations reach same endpoint quicker but with exponentially increased sensitivity, enamel changes, and complication risk. Lower concentrations work but require patience. Individual sensitivity tolerance should guide selection, not marketing pushing highest percentages. Sensitivity risk stratification should determine starting concentration with gradual increase if tolerated. No previous sensitivity: Start 10% hydrogen or 20% carbamide peroxide. Mild sensitivity history: Begin 6% hydrogen or 15% carbamide. Moderate sensitivity: Use 3-4% hydrogen or 10% carbamide. Severe sensitivity: Consider non-peroxide alternatives or avoid whitening. Exposed roots contraindicate whitening regardless. This individualized approach prevents unnecessary suffering from overly aggressive protocols.Concentration selection by patient:
- Virgin teeth, no sensitivity: 10% HP/20% CP
- Previous whitening, mild sensitivity: 6% HP/15% CP
- Sensitive teeth: 3-4% HP/10% CP
- Severe sensitivity: Avoid or alternatives
- Teenagers: Lower concentrations mandatory
- Aggressive goals: Extended time, not higher percentage
Sensitivity Prevention and Management
Preventing sensitivity proves far superior to treating after occurrence, with proper protocols reducing incidence 70% while enabling comfortable whitening for sensitive patients. Desensitizing toothpaste containing potassium nitrate used 2-4 weeks before whitening decreases tubule responsiveness. Fluoride varnish application creates protective barrier. Starting with lower concentrations allows adaptation. Shorter initial sessions test tolerance. These preventive measures transform painful experiences into tolerable treatments. Potassium nitrate and fluoride protocols significantly reduce whitening sensitivity through different mechanisms. Potassium nitrate penetrates tubules decreasing nerve excitability. 5% concentration in toothpaste or gel proves effective. Fluoride occludes tubules and strengthens enamel. Varnish application before whitening helps. Combined use provides synergistic protection. Two weeks pre-treatment use recommended minimum. According to clinical skincare research, proper desensitization enables 90% of sensitive patients to whiten comfortably.Sensitivity prevention protocol:
- Weeks -4 to -2: Desensitizing toothpaste
- Week -1: Fluoride varnish application
- Day 0: Lower concentration start
- During: Shorter sessions initially
- Between: Potassium nitrate gel
- After: Continued desensitizing care
Realistic Expectations and Maintenance
Setting appropriate expectations requires honest discussion about achievable results based on individual factors rather than showing best-case marketing materials. Most patients achieve 2-5 shade improvement, not 8-10 advertised. Natural teeth cannot match porcelain white. Yellow responds better than gray. Young teeth whiten better than old. Some stains won’t budge regardless. This reality check prevents disappointment while establishing achievable goals worth pursuing. Shade improvement depends on starting point with darker teeth showing more dramatic change. A4 to A2 appears more impressive than A2 to A1 despite equal shade movement. Very dark teeth may need multiple rounds. Already light teeth show minimal change. Gray tones respond poorly. Tetracycline stains lighten but persist. According to dermatology research, realistic planning based on starting shade and stain type predicts satisfaction better than promising maximum results.Realistic outcome expectations:
- Yellow teeth: 3-5 shades typical
- Gray teeth: 1-2 shades maximum
- Mixed staining: Variable response
- Young patients: Better results
- Heavy staining: May need multiple rounds
- Intrinsic stains: Lighten but remain visible
Special Considerations and Contraindications
Certain conditions absolutely contraindicate whitening while others require modified protocols, yet screening remains inadequate with providers treating inappropriate candidates who face complications. Pregnancy and nursing contraindicate elective whitening. Allergies to peroxide preclude treatment. Severe sensitivity needs resolution first. Extensive restorations won’t match. Active decay requires treatment. Gum disease needs control. These contraindications protect patient safety despite lost revenue. Medical conditions affecting whitening safety or efficacy need careful consideration. Temporomandibular disorders worsen with tray wear. Gastroesophageal reflux erodes enamel increasing sensitivity. Bulimia creates severe erosion contraindication whitening. Xerostomia reduces remineralization capacity. Immunosuppression affects healing. Cancer treatment causes mucositis. These conditions modify or prevent safe whitening despite patient desires.Contraindications and precautions:
- Absolute: Pregnancy, allergy, severe decay
- Relative: Sensitivity, recession, erosion
- Medical: TMD, GERD, eating disorders
- Dental: Extensive restorations, active disease
- Age: Under 14 contraindicated
- Behavioral: Unrealistic expectations
MD Spa’s Professional Whitening Excellence
Comprehensive Shade Assessment
MD Spa performs detailed tooth color evaluation beyond simple shade tab comparison, using digital photography, spectrophotometer measurement, and individualized assessment identifying realistic whitening potential. Initial consultation examines existing shade distribution, stain types, enamel condition, and limiting factors. This thorough evaluation prevents inappropriate treatment while establishing achievable goals based on individual biology rather than marketing promises. Digital shade mapping documents baseline color variation across smile. Central incisors typically lightest. Canines appear yellower. Cervical areas darker than incisal. This variation means uniform ultra-white impossible. Photography under standardized conditions enables accurate comparison. Spectrophotometer provides objective measurement beyond subjective vision. Multiple measurements ensure accuracy. According to clinical skincare research, objective measurement improves outcome prediction 40% over visual assessment.Assessment components performed:
- Visual shade evaluation
- Digital photography documentation
- Spectrophotometer measurements
- Stain type identification
- Enamel quality assessment
- Restoration inventory
- Sensitivity screening
Customized Treatment Protocols
MD Spa develops individualized whitening plans based on assessment findings rather than applying one-size-fits-all protocols. Sensitive patients start with lower concentrations. Resistant stains may need multiple rounds. Quick results for events use in-office treatment. Budget-conscious receive at-home options. This customization achieves optimal outcomes within individual constraints rather than forcing inappropriate standard protocols. Concentration selection matches patient tolerance and goals. No sensitivity allows standard 10% hydrogen peroxide. Mild sensitivity starts 6% with gradual increase. Severe sensitivity uses 10% carbamide overnight. Teenagers receive reduced concentrations. Results timeline determines aggressive versus conservative approach. The treatment safety protocols support individualized protocols over standardized treatments.Protocol customization factors:
- Sensitivity level determining concentration
- Timeline influencing intensity
- Budget affecting modality
- Age requiring adjustment
- Stain type guiding approach
- Lifestyle indicating maintenance
Advanced Application Techniques
MD Spa employs precise application methods maximizing efficacy while protecting soft tissues from chemical burns common with careless technique. Proper isolation using barriers prevents gum irritation. Even gel distribution ensures uniform whitening. Appropriate volume prevents waste and overflow. Careful monitoring identifies problems immediately. These technical refinements transform basic peroxide application into professional medical treatment. Isolation techniques prevent soft tissue damage while ensuring gel remains on teeth. Liquid dam creates protective barrier. Proper placement seals margins completely. Cotton roll isolation absorbs excess. Gauze protects lips and tongue. Suction removes pooled saliva diluting gel. This meticulous protection enables higher concentrations safely. The dermatology research confirms proper isolation prevents 95% of soft tissue complications.Application technique elements:
- Complete soft tissue isolation
- Even gel distribution
- Appropriate volume per tooth
- Prevention of pooling
- Regular monitoring during treatment
- Immediate intervention if problems
Long-Term Maintenance Programs
MD Spa’s whitening programs extend beyond initial treatment through maintenance protocols preserving results and preventing rapid restaining. Touch-up schedules individualize based on lifestyle and staining rate. Chromogen exposure counseling reduces restaining. Professional cleanings remove accumulation. Annual reassessment adjusts protocols. This comprehensive approach maintains investment value long-term. Maintenance scheduling prevents complete relapse requiring retreatment from baseline. Quarterly touch-ups for heavy stainers. Biannual for moderate chromogen exposure. Annual for minimal staining lifestyle. Custom trays enable affordable home maintenance. Professional boost sessions when needed. This proactive approach maintains brightness efficiently. The skin aging science shows consistent maintenance extends results 200% versus sporadic retreatment.Maintenance program components:
- Initial maximum whitening
- Customized touch-up schedule
- Lifestyle modification counseling
- Professional cleaning intervals
- Annual shade reassessment
- Tray replacement as needed
Frequently Asked Questions
“Hollywood white” represents porcelain veneers or crowns, not natural teeth, as biological enamel cannot achieve the opacity and brightness of ceramic restorations regardless of whitening aggressiveness. Natural teeth have translucent enamel over yellow dentin creating depth and vitality but limiting maximum whiteness. Attempting to reach porcelain white through excessive bleaching causes irreversible enamel damage and pulp death. Celebrities displaying toilet-bowl white smiles have veneers costing $20,000-$60,000, not whitened natural teeth. According to dermatology research, maximum safe whitening achieves A1 or B1 shade at best, nowhere near the artificial white of porcelain, making Hollywood white physically impossible for natural teeth regardless of treatment intensity or cost.
Higher peroxide concentrations don’t whiten better—only faster with exponentially increased sensitivity—making moderate concentrations with patience superior for identical results with comfort. Studies consistently demonstrate 10% hydrogen peroxide achieves maximum whitening potential with additional concentration only accelerating timeline. 35% hydrogen peroxide reaches same endpoint as 10% but in hours versus days, causing severe sensitivity lasting weeks. The clinical skincare research proves saturation point exists where more peroxide provides zero additional benefit, only unnecessary trauma, making paying premium for high-concentration treatments wasteful for those who can achieve identical results gently with time.
LED lights and “laser” whitening represent marketing theater adding zero whitening benefit according to multiple controlled studies comparing peroxide alone versus peroxide with lights. Blue LED cannot generate heat necessary for chemical acceleration. True lasers risk thermal damage without improving outcomes. The peroxide performs all actual whitening while lights create perception of advanced technology justifying premium pricing. According to treatment safety protocols, modern optimized peroxide formulations work maximally without any light activation, making $200-$400 light add-ons pure profit margin through technological deception rather than improve results.
Whitening increases dentinal tubule diameter 200-300% while temporarily demineralizing enamel, creating hydraulic conductivity allowing stimuli to trigger nerve responses that normally wouldn’t occur. Temperature changes, sweet foods, acidic drinks, even air cause pain through exposed tubules. Most sensitivity resolves within 1-2 weeks as tubules narrow and enamel remineralizes. However, 5-10% develop persistent sensitivity from excessive treatment causing irreversible pulp inflammation. The aesthetic medicine guidelines emphasize proper protocols prevent most sensitivity, but once occurred requires immediate discontinuation, desensitizing treatments, and possible endodontic evaluation if persisting beyond two weeks.
Realistic whitening achieves 2-5 shade improvement for most patients, with yellow tones responding better than gray, young teeth whitening more than old, and results lasting 6-24 months depending on lifestyle maintenance. Starting at typical A3 shade, reaching A1 represents excellent result—B1 possible for some but not lighter. Gray intrinsic stains may lighten one shade maximum. Results inevitably decline as chromogen exposure restains teeth, requiring touch-ups every 6-12 months maintaining improvement. According to skin aging science, accepting natural variation and maintaining realistic expectations while committing to ongoing maintenance provides sustainable satisfaction, versus pursuing impossible ultra-white requiring dangerous overtreatment with disappointing temporary results.